Como ya sabes por nuestras entradas anteriores, la lactosa es la principal fuente de azúcar de la leche y de los productos lácteos. También está presente en algunos productos industriales en forma de conservante o aditivo. La podemos encontrar en carnes procesadas como salchichas o patés, margarinas, helados, salsas, algunos fiambres y embutidos, cereales enriquecidos, sopas instantáneas, alimentos y comidas preparadas, medicamentos, etc. Es decir, la lactosa está presente no sólo en la leche sino también en una gran cantidad de productos que consumimos a diario.
Es fundamental no confundir el significado de la intolerancia la lactosa (IL) con el de la malabsorción (MAL) de la misma. No solo es básico para tener claras las diferencias de ambas patologías, sino que el abordaje del tratamiento es completamente distinto y es vital conocer lo que uno padece para poder solucionarlo.
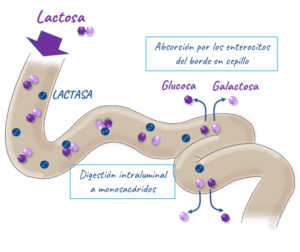 Cuando hablamos de que una persona es intolerante a la lactosa, hacemos referencia al defecto en la fabricación de la enzima de la lactasa, que como ya se ha descrito en posts anteriores, es la encargada de disociar la lactosa en galactosa y glucosa, que ocurre de manera normal en el intestino delgado. Para que nuestro organismo absorba correctamente la lactosa, la actividad de esta enzima debe ser adecuada, debido a que el organismo sólo puede absorber azúcares simples.
Cuando hablamos de que una persona es intolerante a la lactosa, hacemos referencia al defecto en la fabricación de la enzima de la lactasa, que como ya se ha descrito en posts anteriores, es la encargada de disociar la lactosa en galactosa y glucosa, que ocurre de manera normal en el intestino delgado. Para que nuestro organismo absorba correctamente la lactosa, la actividad de esta enzima debe ser adecuada, debido a que el organismo sólo puede absorber azúcares simples.
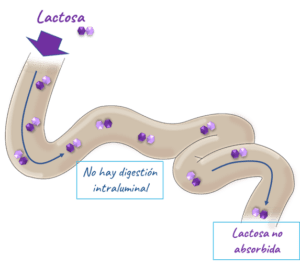
El intolerante a la lactosa al carecer de esta encima, no produce la digestión de la lactosa, por lo que llega intacta al colon en vez de ser digerida en el intestino delgado.
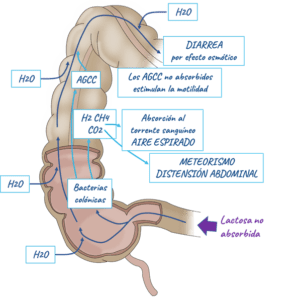
En el colon, las bacterias colónicas fermentan esta lactosa. Es aquí donde pueden ocurrir dos situaciones diferentes.
- Por un lado, si a pesar de haberse producido una malabsorción en el intestino delgado, estamos ante un individuo con una microbiota sana en el colon, la lactosa sin digerir se metabolizará. Por lo tanto estaríamos ante un individuo que es mal absorbedor de la lactosa, sin embargo gracias a su microbiota, no padece ningún síntoma asociado.
- Por otro lado, si estamos ante un individuo con una microbiota desequilibrada en el colon, al llegar y producirse la fermentación de la lactosa, se generara una elevada cantidad de gases, síntomas de distensión abdominal, diarrea o estreñimiento, dolor … entre otros, pero también pueden aparecer síntomas extra-digestivos como dolor de cabeza, fatiga crónica, debido al estado inflamatorio interno. Estaríamos ante un caso de intolerante a la lactosa.
Ser intolerante a la lactosa no es irreversible, ya que se puede solucionar temporalmente tomando una pastilla de lactasa, para poder ingerir alimentos con lactosa, pero no es un tratamiento al déficit, carencia o mal funcionamiento de esta encima. Sin embargo, como tolera tu microbiota la lactosa es algo que nosotros en cierta medida mismos podemos cuidar. Está demostrado que el descanso digestivo en horas de oscuridad, el ejercicio físico aeróbico, la gestión del estrés, alimentarse de una manera equilibrada y el uso de prebióticos mejora la microbiota notablemente.
Por tanto, la absorción de la lactosa, es lo que determinará si el individuo es buen o mal absorbedor, se produce a nivel de intestino delgado, gracias o en consecuencia a la enzima de la lactasa. Así si no hay absorción de la lactosa y estamos ante un individuo con una a microbiota alterada diagnosticamos una intolerancia a la misma, que lleva consigo todos los síntomas asociados.
Por lo que un individuo puede ser mal absorbedor de la lactosa por no tener la capacidad de disociarla en sus monosacáridos y sin embargo ser tolerante a la misma por tener una microbiota sana y por tanto poder consumir este azúcar. Así como puede haber un individuo, que teniendo la capacidad de absorber la lactosa, ser intolerante debido al estado de su microbiota, y que a la larga resolviendo el problema con sus bacterias y o arqueas colónicas poder tolerar la lactosa sin ningún problema asociado.