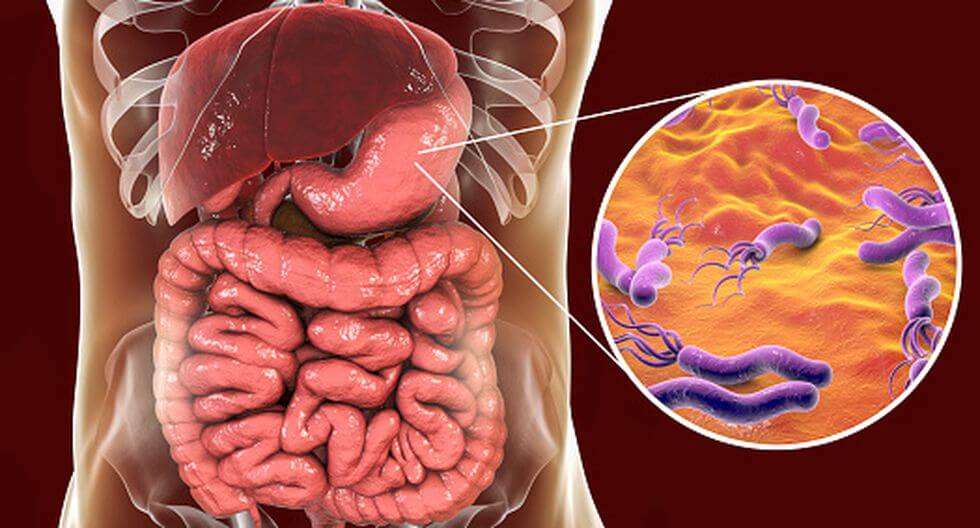
Helicobacter pylori es un bacilo Gram negativo altamente móvil, con forma de espiral y está rodeado por flagelos. Fue aislado por primera vez en el año 1983 por Robin Warren y Barry Marshall, que lo relacionaron con la aparición de úlceras gástricas, descubrimiento por el que les fue concedido el Premio Nobel de Medicina en 1995.
En las personas infectadas, Helicobacter vive en la capa mucosa del estómago donde, gracias a su enzima ureasa, produce amoníaco y neutraliza parcialmente el pH ácido natural del estómago, protegiéndose de éste, lo que le permite sobrevivir y proliferar. La bacteria además segrega ciertas proteínas que atraen a los macrófagos y neutrófilos, produciendo inflamación en la zona afectada, es decir, gastritis.
Epidemiología
La infección por Helicobacter pylori es muy común y suele producirse en la infancia, por vía fecal-oral u oral-oral. La prevalencia del Helicobacter pylori varía entre diferentes grupos de población y dentro de un mismo grupo. El riesgo de infección a lo largo de toda la vida en personas de países desarrollados está entre el 40% y el 60%, alcanzando el 90% en los países en vías de desarrollo, en los cuales aproximadamente el 50% de la población ya está infectada a los 10 años de edad. No obstante, sólo un 10-25% de los infectados desarrolla síntomas.
Patologías y complicaciones
Helicobacter pylori se ha asociado a diferentes enfermedades, la mayoría de ellas del tracto digestivo. Su implicación en la gastritis crónica activa, su asociación con la úlcera gastroduodenal y su inclusión por parte de la IARC entre los agentes carcinógenos tipo 1, la ha convertido en uno de los microorganismos de mayor interés en patología humana.
Helicobacter puede provocar complicaciones como:
- Gastritis crónica: proceso inflamatorio más frecuentes en el ser humano y estrechamente relacionado con la infección por pylori.
- Úlcera duodenal y úlcera gástrica: perforaciones de la mucosa del intestino o del estómago, respectivamente.
- Linfoma MALT: es un linfoma que predomina en la edad adulta, más frecuente en mujeres y que constituye el 5-10 % de las neoplasias gástricas.
- Dispepsia no ulcerosa: dolor o molestia crónica recurrente en la parte superior del abdomen.
- Cáncer gástrico: la infección por pylori es considerada un factor de riesgo en el desarrollo del cáncer de estómago.
Síntomas
- Sensación de ardor o acidez en la parte alta del abdomen, bajo el esternón.
- Dolor estomacal.
- Distensión.
- Saciedad precoz.
- Falta de apetito.
- Náuseas y vómitos.
- Oscurecimiento de las heces, pudiendo llegar a ser negras.
- Anemia y cansancio.
¿Tienes alguno de estos síntomas? No lo dejes pasar, el malestar gástrico no es normal. Consulta con tu médico.
Diagnóstico
Para el diagnóstico de Helicobacter pylori, existen diferentes técnicas:
- Test de aliento con urea marcada con 13C: es una prueba no invasiva que consiste en tomar un comprimido de urea marcada. En presencia de pylori, su actividad ureásica degrada la urea liberando amoníaco y CO2 marcado con 13C, que es detectado en la muestra de aire espirado. Además, la prueba es mucho más fiable y sensible si previamente se administra una bebida de ácido cítrico. Esto evita la aparición de falsos negativos.
- Determinación de antígeno en heces: consiste en la recogida de una muestra fecal y su examen para detectar la presencia del antígeno de pyloria mediante el uso de un método diagnóstico llamado ELISA con anticuerpos monoclonales. Cuando los anticuerpos empleados son policlonales, la fiabilidad de la prueba se reduce y son habituales los falsos positivos.
- Test serológico: consiste en la extracción de una muestra de sangre y su análisis para detectar anticuerpos frente a pylori. Sólo se utiliza cuando existe una patología gástrica, como hemorragia, gastritis atrófica o determinados tumores, que puedan alterar la interpretación de las pruebas anteriores.
- Endoscopia digestiva: permite la recogida de una biopsia de la mucosa gástrica y su análisis histológico para detectar la actividad ureasa o bien para identificar microscópicamente la presencia de la bacteria. Sin embargo, es una técnica invasiva y su sensibilidad no es demasiado elevada, puesto que la muestra de tejido puede no contener la bacteria.
Tratamiento
Su médico será quien determine el tratamiento en base a las características del paciente. No obstante, el objetivo siempre es erradicar la bacteria, por lo que el tratamiento suele ser una terapia antibiótica. Sin embargo, H. pylori ha desarrollado resistencia a varios antibióticos, por lo que a veces su eliminación no se produce al 100% y es necesario repetir el tratamiento con una terapia antibiótica diferente.
Es importante realizar de nuevo un test diagnóstico después del tratamiento para confirmar la erradicación de Helicobacter pylori. Solicítalo a tu médico.
Bibliografía
- Forman D. The prevalence of Helicobacter pyloriinfection in gastric cancer. Pharmacol. Ther. 1995;9 Suppl 2:71-6.
- Kuipers EJ, Thijs JC, Festen HP. The prevalence of Helicobacter pyloriin peptic ulcer disease. Pharmacol. Ther. 1995;9 Suppl 2:59-69.
- Gisbert JP, Pajares JM. Review article: 13C-Urea breath test in the diagnosis of Helicobacter pyloriinfection: a critical review. Pharmacol. Ther. 2004 Nov. 15;20 (10):1001-17.
- Gisbert JP, Pajares JM. 13C-Urea breath test in the management of Helicobacterpylori Dig Liver Dis 2005 Dec; 37 (12):899-906.
- Logan R.P.H. Urea Breath test in the management of Helicobacterpylori Gut 1998;43 Suppl. 1:S47-S50.
- Parente F, Bianchi Porro G. The 13C-Urea breath test for non-invasive diagnosis of Helicobacterpylori infection: which procedure and which measuring equipment? Eur J Gastroenterol Hepatol 2001. July 13 (7):803-806.
- Gisbert JP, Ducons J, Gomollón F, Domínguez-Muñoz JE, Borda F, Miño G, Jiménez I, Vázquez MA, Santolaria S, Gallego S, Iglesias J, Pastor G, Hervás A and Pajares JM. Validation of the 13C-Urea breath test for the initial diagnosis of Helicobacterpylori infection and to confirm erradication after treatment. Rev Esp Enferm Dig 2003; 95 (2):121-126.
- Bazzoli F. et al. Validation of the 13C-Urea breath test for the diagnosis of Helicobacterpylori infection in children: a multicenter study. Am J Gastroenterol 2000; 95: 646-650.
- Canete A, Abunaji Y, Alvarez-Calatayud G, DeVicente M, González-Holguera JA, Leralta M, Pajares JM, Gisbert JP. Breath test using a single 50-mg dose of 13C-Urea to detect Helicobacterpylori infection in children. J Pediatr Gastroenterol Nutr 2003 Jan;36 (1):105-11.
- Leodolter A, Armin U, Domínguez Muñoz JE, Malfertheiner P. Less Sensitivity of the 13C-Urea breath for the diagnosis of Helicobacterpylori infection by using orange juice as test drink. Gut 1997;40: 459-462.